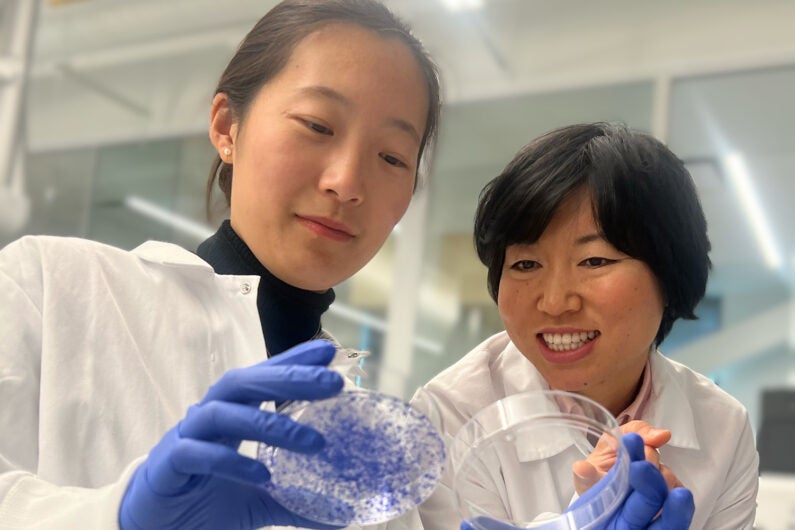
Songnan Wang (left) and Lingyin Li (right) found that a protein called ENPP1 acts as an on/off switch for breast cancer metastases. High protein levels lead to a high chance of metastasis (as seen by cells growing in the dish on the left), while low levels lead to no metastasis (as seen by no cells growing in the dish on the right). (Image credit: Lingyin Li and Songnan Wang)
Despite their promise, immunotherapies fail to treat many cancers, including over 80% of some of the most advanced breast cancers. And many of those patients who do respond still experience metastases eventually. New research from Stanford University and the Arc Institute has revealed a better way to predict and improve patient responses.
A team led by Lingyin Li, associate professor of biochemistry at Stanford and Arc Core Investigator, found that a protein called ENPP1 acts as an on/off switch that controls breast cancer’s ability to both resist immunotherapy and metastasize. The study, published on Dec. 20 in the Proceedings of the National Academy of Sciences, showed that ENPP1 is produced by cancer cells and by healthy cells in and around the tumor, and that high patient ENPP1 levels are linked to immunotherapy resistance and subsequent metastases. The research could lead to new, more effective immunotherapies and help clinicians better predict patient response to existing medicines.
“Our study should offer hope for everyone,” said Li, who is also an institute scholar at Sarafan ChEM-H.
Thawing cold tumors
Immunotherapies, like pembrolizumab (Keytruda), work by blocking an immune-dampening interaction between a cancer cell and a T cell, a kind of immune cell. For this to be effective, though, T cells need to permeate the tumor. So-called “hot” tumors, like those in melanoma and a subset of lung cancer, are treatable through immunotherapies, but many others, like breast and pancreatic cancers, are “cold,” devoid of T cell infiltration.
In her quest to turn cold tumors hot, Li started with cGAMP, a molecule that cells produce when their DNA is damaged, which happens when a cell becomes cancerous. If left intact, cGAMP activates an immune response through what is known as the STING pathway, which can help make a tumor hot. Li previously discovered that cGAMP is exported outside the cells but often, before it can trigger a response, a protein called ENPP1 chews up these molecular “danger” signals. ENPP1, she proposed, helped keep cold tumors cold.
High levels of ENPP1 correlate with poor prognosis in many cancers, but the protein can perform many actions in the body, so Li set out to determine if its cGAMP-chewing ability is behind its clinical significance.
An on/off switch
Li began collaborating with two professors at the University of California, San Francisco: Hani Goodarzi, also an incoming Arc Institute Core Investigator, and Laura Van’t Veer, a clinician who leads the I-SPY 2 Trial, a groundbreaking breast cancer trial. ENPP1 levels naturally vary across individuals, so the team looked at data from patients in the I-SPY 2 Trial to see how responses to pembrolizumab varied with ENPP1 levels at the time of diagnosis.
The results were astounding. Patients with high ENPP1 levels had low response to pembrolizumab and high chance of metastases. Those with low ENPP1 levels had a high response to pembrolizumab and no metastases. ENPP1 predicted both response to immunotherapy and likelihood of relapse.
Two things were suddenly clear: that ENPP1 was critical in metastases, not just in primary tumors; and that they should be looking at ENPP1 in healthy cells, not only in cancer cells.
“Using the finest molecular scalpels developed in our lab, I was excited to dig deeper and figure out exactly how ENPP1 has such a dramatic influence on clinical outcomes,“ said Songnan Wang, an MD-PhD student in biochemistry, Arc researcher, and first author on the paper.
In a series of mouse studies, Wang proved that removing ENPP1 entirely or eliminating only its cGAMP-chewing ability in normal and cancer cells yielded exactly the same result: decreased tumor growth and decreased metastases. And the team proved that it resulted directly from suppressing the STING pathway. They found an on/off switch.
On top of the waterfall
Immune pathways are often described as “cascades” with a series of signals that trigger downstream actions that eventually lead to a response.
“For cancers to stop the immune system from detecting them, they need to build dams that block the signal from flowing,” said Li. “We have shown that ENPP1 acts like a big dam at the top of the waterfall.”
This means that clinicians can use ENPP1 levels to better determine appropriate treatment for breast cancer patients. It also means that drugs that destroy the ENPP1 dam could make existing therapies more effective – and several ENPP1 inhibitors are already in clinical development.
While this work focused on breast cancer, Li believes that ENPP1 plays a critical role in other kinds of “cold” tumors.
“I hope to inspire clinicians who treat cancers – including lung cancer, glioblastoma, and pancreatic cancer – to investigate ENPP1’s role in patient outcomes,” said Li.
Li is also a member of Stanford Bio-X and the Stanford Cancer Institute. Other Stanford co-authors include Alby Joseph and Valentino Sudyaryo (of Stanford and Arc); Volker Böhnert, Gemini Skariah, and Xuchao Lyu (of Stanford). Additional co-authors are from the University of California, San Francisco, and Arc.
This work was supported by the Arc Institute, the Stanford Chi-Li Pao Foundation Alpha Omega Alpha Student Research Fellowship, the Stanford Medical Scholars Research Program, a Stanford Graduate Fellowship, the Chemistry/Biology Interface (CBI) Predoctoral Training Program at Sarafan ChEM-H, the NSF Graduate Research Fellowship Program, an Era of Hope Scholar Award, an NIH New Innovator Award, a Pew-Steward Scholars for Cancer Research award, and the National Institutes of Health.
Lingyin Li and Volker Böhnert have filed two patents on ENPP1 inhibitors (PCT/US2020/015968 and PCT/US2018/050018) that are licensed to Angarus Therapeutics. Li is a co-founder of Angarus Therapeutics.
