A new study showed that Vitamin D supplementation can reduce heart attacks by 52%. This is important since heart attacks are the #1 cause of death, about one billion people worldwide are deficient in Vitamin D, and supplementing vitamin D is cheap.
TARGET-D is a randomized trial in people with who previously had a heart attack, presented at American Heart Association (AHA) Scientific Sessions. In the study, they measured vitamin D blood levels every 3 months, and adjusted vitamin D3 doses to keep vitamin D levels within a target range of 40–80 ng/mL.
Participants in the experiment arm who stayed within 40-80 ng/mL of vitamin D had a 52% lower risk of a repeat heart attack.
Why would that be? Vitamin D is not part of the standard six biomarkers for cardiovascular health (blood pressure, ApoB, Lp(a), hs-CRP, eGFR, and A1c) that we’ve written about extensively here.
In the rest of this post, we’ll try to explain why. We’ll cover the physiological mechanisms that link Vitamin D₃ and D₂ to heart health, how to measure vitamin D, specific ways to get more vitamin D, and potential future work.
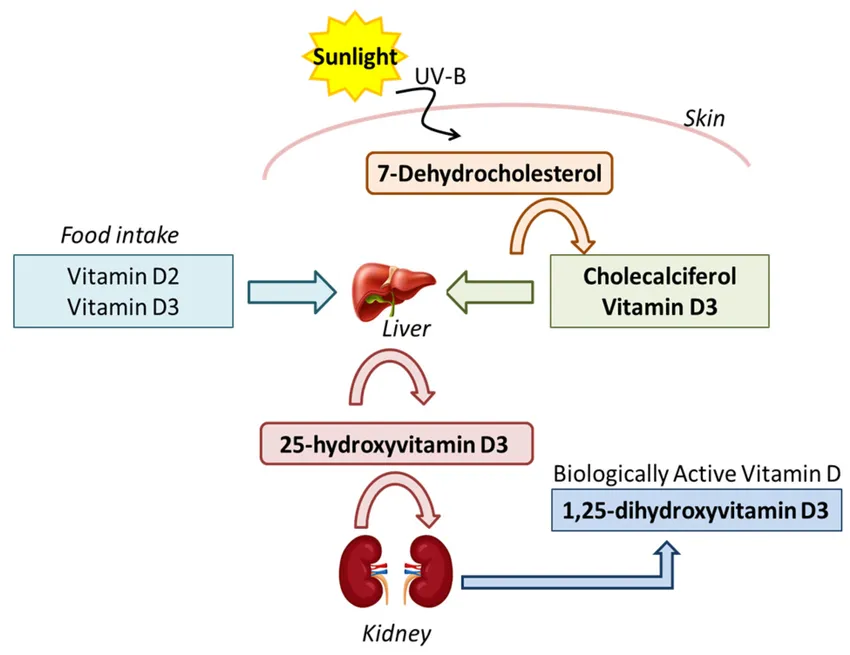
Vitamin D comes in two main forms. Vitamin D₃ (cholecalciferol) is made in your skin when UVB sunlight hits it, and also in animal foods. Vitamin D₂ (ergocalciferol) is from plants and fungi.
Neither is active on its own, but is converted by the liver and kidneys into a calcitriol, a form that binds to Vitamin D receptors in the nucleus of many cells.
 Multiple chemical pathways absorb or create vitamin D.
Multiple chemical pathways absorb or create vitamin D.
Vitamin D then regulates hundreds of genes with broad effects. It increases calcium absorption in the intestines (children without vitamin D get rickets). It regulates adaptive immunity (inflammation). It regulates blood pressure through effects on the renin-angiotensin system.
Vitamin D also stabilizes plaques in arteries by reducing macrophage activation. Plaque is the buildup of fats (e.g., cholesterol), immune cells (Macrophages, T-lymphocytes), calcium, and a few other components. Soft plaques have more inflammatory cells and are more vulnerable to rupture. When plaque ruptures and travels to the point where it blocks a coronary artery, that causes a heart attack.
 One mechanism is that Vitamin D stabilizes plaques by reducing inflammatory cells. Other mechanisms include calcium and blood pressure regulation
One mechanism is that Vitamin D stabilizes plaques by reducing inflammatory cells. Other mechanisms include calcium and blood pressure regulation
One way to think about this: vitamin D doesn’t prevent heart disease from starting, but may reduce the chance that existing disease suddenly turns into another heart attack.
Vitamin D levels are measured with a 25-hydroxyvitamin D blood test (sometimes written as 25(OH)D).
In the U.S., results are reported in ng/mL. The TARGET-D study aimed for a 40–80 ng/mL range, which is higher than the threshold for “deficiency” but within a safe range for most adults.
An Empirical Health membership includes vitamin D testing along with a suite of cardiovascular and nutritional biomarkers (cholesterol, ApoB, Lp(a), hs-CRP, ferritin, eGFR, and more).
 There are many sources of vitamin D: food, supplements, sunlight.
There are many sources of vitamin D: food, supplements, sunlight.
Most of use could use more vitamin D.
- Sunlight: Your skin makes vitamin D when exposed to UVB rays from the sun. Even short periods (10-30 minutes with arms and legs exposed) can be enough for many people.This depends on your skin tone, where you live, and the season.
- Food sources: Fatty fish (like salmon, mackerel, sardines), egg yolks, cod liver oil, and fortified foods (milk, orange juice, some cereals) provide vitamin D. However, diet alone is rarely enough to reach optimal blood levels.
- Supplements: Vitamin D3 (cholecalciferol) is the preferred supplemental form. Typical doses range from 1,000 to 4,000 IU per day, but individual needs vary.
There are two main caveats to the TARGET-D study. First, this was presented at the American Heart Association scientific sessions, but the full manuscript isn’t out yet. It’s possible the results will end up not being statistically significant, having a methodological flaw, and so on. In the presented results, the reduction in heart attack risk was statistically significant but the change in overall death and stroke risk had a p value > 0.05. Second, while Vitamin D seems to be an effective intervention to reduce heart attack risk, we don’t yet know whether Vitamin D is an independent marker of heart disease risk or whether it’s reflecting known mechanisms such as inflammation and calcification.
In a randomized control trial, adjusting vitamin D supplement dosages based on blood test results led to a 52% reduction in heart attacks. If confirmed in further research, optimizing vitamin D could join cholesterol and blood pressure as a key intervention for reducing heart attack risk, especially for people with a history of heart disease.
Get your free 30-day heart health guide
Evidence-based steps to optimize your heart health.